Mouth Breathing: Physical, Mental and Emotional Consequences
March 9, 2017 | by P. McKeown; M. Macaluso | OralHealthGroup.com
Breathing is one of the most vital functions of the human body. Every breath we take can have a positive or negative impact on our bodies depending on how it is performed; and it has been well established that normal breathing should be achieved through the nose. However, it may be detoured to the oral cavity in the presence of an airway obstruction. 35
During normal breathing, the abdomen gently expands and contracts with each inhalation and exhalation. There is no effort involved, the breath is silent, regular, and most importantly, through the nose. Abnormal breathing or mouth breathing on the other hand; is often faster than normal, audible, punctuated by sighs, and involves visible movements of the upper chest. This type of breathing is normally only seen when a person is under stress, but for those who habitually breathe through their mouths, the negative side effects of stress and over-breathing become chronic. Habitual mouth breathing has serious implications on an individual’s lifelong health, including the development of the facial structures. This article explores the benefits of nasal breathing over mouth breathing, and provides a self-help exercise to help decongest the nose.
1. Nasal breathing and the Importance of Nitric Oxide
Nasal breathing has been well documented to providing various benefits. The nose is equipped with a complex filtering mechanism which purifies the air we breathe before it enters the lungs. 11 Breathing through the nose during expiration helps maintain lung volumes and so may indirectly determine arterial oxygenation. 28
One of the most important reasons for nasal breathing, is due to the production of nitric oxide (NO). 9 NO exists in the human breath, but little is known about its site of origin or enzyme source. Most NO in normal human breath derives locally from the nose where it can reach high levels during breath-holding. 39 This incredible molecule, is said to be produced in mammalian cells by specific enzymes and is believed to play a vital role in many biological events including regulation of blood flow, platelet function, immunity, and neurotransmission. 18 Although this gas is produced in minute amounts, when it is inhaled through the nose into the lungs, it will follow the airstream to the lower airways and the lungs where it aides in increasing arterial oxygen tension; hence enhancing the lungs capacity to absorb oxygen. 18 Nitric Oxide also plays an important role in reducing high blood pressure, maintaining homeostasis, immune defense and neurotransmission. 6
2. Effects of Mouth Breathing
Habitual mouth breathing, conversely involves an individual breathing in and out through the mouth for sustained periods of time, and at regular intervals during rest or sleep.
It is well documented that mouth breathing adults are more likely to experience sleep disordered breathing, fatigue, decreased productivity and poorer quality of life than those who nasal-breathe. 16,22,23 In children, the harmful effects of mouth breathing are far greater, since it is during these formative years that breathing mode helps to shape the orofacial structures and airways.
Children whose mouth breathing is left untreated for extended periods of time, can set the stage for lifelong respiratory problems and including, a less attractive face to name a few. As a result, malocclusions such as a skeletal Class II or Class III, along with a long lower face height (characterized as “long face syndrome”), and high palatal vaults may also be noted. 14 These resultant craniofacial alterations associated with mouth breathing can significantly aggravate or increase the risk of snoring and obstructive sleep apnea in both children and adults.
A study conducted by Fitzpatrick et al, demonstrated the critical role of the soft palate in determining oral or nasal airflow. The study showed that during mouth breathing, the soft palate will tend to move posteriorly against the posterior pharyngeal wall, thus closing the nasopharyngeal airway. Whereas, during nasal breathing, the soft palate moves inferiorly and anteriorly until it lays against the dorsum of the tongue, thus closing the oropharyngeal airway.
The opening of the mouth during sleep in normal subjects and in patients with obstructive sleep apnea was also documented in this study. Mouth opening, even in the absence of oral airflow, has been shown to increase the propensity to upper airway collapse. The two most likely explanations for the latter finding are that jaw opening is associated with a posterior movement of the angle of the jaw and compromise of the oropharyngeal airway diameter, and that posterior and inferior movement of the mandible may shorten the upper airway dilator muscles located between the mandible and hyoid and compromise their contractile force by producing unfavorable length-tension relationships in these muscles. 10 Therefore, it is of utmost importance to address mouth breathing accordingly.
Unfortunately, it has been noted that there is a lack of awareness regarding the negative impact of airway obstruction via mouth breathing on normal facial growth and physiologic health; and as a result, may be confused for (ADD) and hyperactivity. 14 According to the National Sleep Foundation, attention deficit hyperactivity disorder (ADHD) is linked to a variety of sleep problems. Children and adults behave differently as a result of sleepiness. Adults usually become sluggish when tired while children tend to overcompensate and speed up. For this reason, sleep deprivation is sometimes confused with ADHD in children. Children may also be moody, emotionally explosive, and/or aggressive as a result of sleepiness. In a study involving 2,463 children aged 6-15, children with sleep problems were more likely to be inattentive, hyperactive, impulsive, and display oppositional behaviors. 35,37,5
Another study published in the International Journal of Pediatrics investigating the long-term changes to facial structure caused by chronic mouth breathing noted that this seemingly ‘benign’ habit “has in fact immediate and/or latent cascading effects on multiple physiological and behavioral functions.” 29 Therefore, with this in mind, mouth breathing can have a tremendous impact on the mental and physical health of children; as it can be associated with the restriction of the lower airways, poor quality of sleep, reduced cognitive functioning and a lower quality of life. 5
3. Prevalence, Causes and Physical Manifestations of Mouth Breathing
Brazilian researchers investigating the prevalence of mouth breathing in children ages three to nine found that a 55% random selection of 370 subjects were mouth-breathers. 2 Reported causes of mouth breathing included: allergic rhinitis (81.4%), enlarged adenoids (79.2%), enlarged tonsils (12.6%), and obstructive deviation of the nasal septum (1.0%). The main clinical manifestations of mouth-breathers were: sleeping with the mouth open (86%), snoring (79%), itchy nose (77%), drooling on the pillow (62%), nocturnal sleep problems or agitated sleep (62%), nasal obstruction (49%), and irritability during the day (43%). 3 Although allergic rhinitis is considered one of the leading causes of respiratory obstruction; it is of utmost importance to note that upon the first onset of nasal congestion, a feeling of air deprivation occurs, causing the individual to switch to mouth breathing. 4
Another study conducted by Pereira et al, demonstrated that orofacial changes were noted in mouth breathers such as: half-open lip and lower tongue position, lip, tongue and cheek hypo-tonicity, and tongue interposition between the arches during deglutition and phonation. 26
3.1 Effect of Low Tongue Position
A mouth breather carries the tongue in a low downward position, creating an airspace which allows the person to breathe more freely; and as a result it can lead to abnormal tongue activity. This abnormal tongue activity, can exert an excessive force upon the dentition during swallowing, contributing to malocclusions in children; and leading to periodontal disease and atypical myofascial pain in adulthood. 12,33 This displacing force and misdirection of the tongue, can additionally contribute to microscopic changes in the attachment apparatus; leading to increased tooth mobility and advancing periodontal disease.
Furthermore, this low tongue resting posture can contribute to various morphological changes to the orofacial structures; and consequently, Orofacial Myofunctional Disorders (OMDs) may develop as well. “OMDs are disorders pertaining to the face and mouth and may affect, directly and indirectly, chewing, swallowing, speech, occlusion, temporomandibular joint movement, oral hygiene, stability of orthodontic treatment, facial esthetics, and facial skeletal growth.” 25 The most common forms of OMDs include: oral breathing or lack of habitual nasal breathing; habitual open mouth posture, and lack of lip seal with patent nasal passages; reduced upper lip movement with or without a restricted labial frenum; restricted lingual frenum, from borderline to ankyloglossia; anterior or lateral tongue thrust at rest (static posture); low and forward tongue position at rest, usually accompanied by an increased verticle dimension; inefficient chewing (related or not) to temporomandibular joint (TMJ) disorders or malocclusion; atypical swallowing, with or without a tongue thrust (dynamic posture); oral habits; and forward position of the head at rest, during chewing and during swallowing to name a few. 25
The resting posture of the tongue plays a pivotal role since its effects are far more constant than atypical swallowing. Mouth breathing encourages incorrect positioning of the tongue (on the floor of the mouth), while nasal breathing naturally places the tongue in its proper resting position (on the roof of the mouth), and most important of all aides in achieving a lip seal.
A study conducted by Schmidt et al, indicated that correct tongue resting position (on the roof of the mouth) resulted in a significant activity in the temporalis and suprahyoid muscles as well as a significant reduction in heart rate variability when compared with a low tongue resting position (on the floor of the mouth). 27 In other words, a proper tongue resting posture is essential for achieving orofacial balance.
3.2 Postural Problems
In addition to abnormal swallowing patterns and facial characteristics, postural problems may also be present in those who habitually breathe through their mouth. Mouth breathers tend to assume a characteristic posture, carrying their heads forward in order to compensate for the restriction to their airways and make breathing possible.
A study conducted by Okuro et al, demonstrated how the respiratory biomechanics and exercise capacity were negatively affected by mouth breathing; and that the presence of moderate forward head posture acted as a compensatory mechanism in order to improve respiratory muscle function. 24 This forward head posture often leads to muscle fatigue, neck pain, tension in the temporomandibular joint area, spinal disc compression, early arthritis, tension headaches, and dental occlusal problems. 8
4. Multidisciplinary approach
In order to achieve proper oronasal balance, a patient must be examined as a whole in a multidisciplinary approach. “It is of fundamental importance to obtain information from the parents/guardians during the medical interview. Therefore, questions about the child’s sleep patterns, if he/she sleeps with the mouth opened, if there is noisy breathing, if the child lacks concentration at school, if the child feels sleepy during the day, if the pillow is wet in the morning; these questions should all be recorded, because they represent important elements in the diagnosis of oral breathing.” 38 Although there is no discernible test to identify mouth breathing, simply observing an individual’s resting breathing habits for at least three minutes can form part of a diagnosis for both children and adults.
It is important to note that an accurate diagnosis of mouth breathing cannot be done with data alone. Therefore, it is recommended to also carry out the Glatzel metal plate test and the time through which the child keeps water in her/his mouth with the lips sealed and without swallowing it, since the results may differ and complete each other. 38
A team of qualified professionals such as Pediatricians, Ear Nose and Throat Doctors, Orthodontists, Dentists, Dental Hygienists, Myofunctional Therapists, Buteyko Breathing Specialists, and Speech Pathologists to name a few; can help arrest the cascading effects associated with mouth breathing.
Management of Nasal Congestion
Proper management and early detection of nasal congestion is key to arresting mouth breathing in an individual. As previously stated, mouth breathing can be a result of various origins associated with respiratory obstruction; such as allergic rhinitis.
Therefore, with rhinitis being one of the leading causes of nasal obstruction, some of the most common treatments used for treating rhinitis include: trigger avoidance, decongestants, corticosteroids or allergy shots. While these offer some therapeutic benefits; for some, they may be effective only for as long as treatment continues. Meanwhile, the individual becomes accustomed to breathing through their mouth and will likely continue this habit even after their nasal airways have cleared, causing a vicious cycle of recurrent congestion. While it may seem counterintuitive nasal breathing is essential for decongesting the nose, along with breathing exercises designed to open the airways, such as the Buteyko Breathing Method.
The Buteyko Method, developed in the 1950s by Russian respiratory physiologist Dr. Konstantin Buteyko, was subject to a study investigating its effectiveness for the treatment of chronic rhinitis in asthma. The study validated evaluations, including the Sinonasal Outcome Test (SNOT); which showed a 71% reduction of rhinitis symptoms at the three month follow up. 1
The Buteyko Breathing Method features a measurement appraisal known as the Control Pause, a breath hold exercise to unblock the nose, and reduced breathing exercises to reset breathing volume towards normal. 19
Nasal Decongestion Exercise
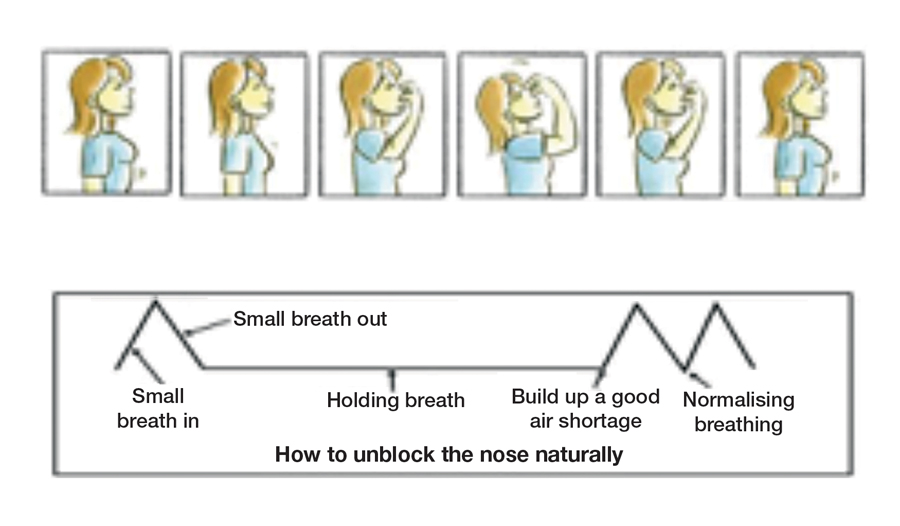
The nose can be unblocked for both allergic and non-allergic rhinitis by performing a breath hold as follows:
- Take a small, silent breath in and let a small, silent breath out through your nose;
- Pinch your nose with your fingers to hold your breath;
- Walk as many paces as possible with your breath held. Try to build up a feeling of air shortage, without overdoing it of course!
- When you resume breathing, do so only through your nose; your breathing must be calmed immediately;
- After resuming your breathing, your first breath is likely to be larger than usual. Calm your breathing as soon as possible by suppressing your second and third breaths;
- You should be able to recover from this breath hold within two to three breaths. If not, you have held your breath for too long;
- Wait for a minute or so and repeat the exercise;
- Repeat this exercise five or six times until the nose is decongested.
In conclusion, it is essential for medical and dental professionals to assess mouth breathing in children and adult patients. If mouth breathing is treated early, its negative effects on facial and dental development, along with the medical and social problems associated with it, can be reduced or averted. 14
As healthcare professionals, we are afforded the perfect opportunity to observe whether patients habitually breathe through their mouths, and to offer practical and effective life-changing recommendations. OH
Oral Health welcomes this original article.
References
1. Adelola O.A., Oosthuiven J.C., Fenton J.E. Role of Buteyko breathing technique in asthmatics with nasal symptoms. Clinical Otolaryngology.2013, April;38(2):190-191 —GENERAL DENTISTRY— 1.
2. Abreu RR1, Rocha RL, Lamounier JA, Guerra AF. Prevalence of mouth breathing among children. J Pediatr (Rio J).2008 SepOct;84(5):467-70.
3. Abreu RR1, Rocha RL, Lamounier JA, Guerra AF.. Etiology, clinical manifestations and concurrent findings in mouth-breathing children. J Pediatr (Rio J).2008;(Nov-Dec;84(6):529-35.
4. Bresolin P, Shapiro G, Shapiro, et al. Mouthbreathing in allergic children, its relationship to dentofacial development. Am. J. Orthod. 83 (1983) 334-340.
5. Borres MP. Allergic rhinitis: more than just a stuffy nose. Acta Paediatrica. 2009 Jul;98(7):1088-92)
6. Chang H R. Nitric Oxide, the Mighty Molecule: Its Benefits for Your Health and Well-Being. 1st ed. United States. ; 2011
7. Conti PB, Sakano E, Ribeiro MA, Schivinski CI, Ribeiro JD. Assessment of the body posture of mouth-breathing children and adolescents. Journal Pediatrics (Rio J). 2011 Jul-Aug;87(4):471-9.
8. Damaging Effects of Forward Head Posture.(2015, January 22). Retrieved from http://www.denvertechchiro.com/files/fhp_revised.pdf
9. Djupesland PG, Chatkin JM, Qian W, Haight JS. Nitric oxide in the nasal airway: a new dimension in otorhinolaryngology. Am J Otolaryngol.2001 Jan; 22(1): 19-32.
10. Fitzpatrick MF, McLean H, Urton AM, Tan A, O’Donnell D, Driver HS. Effect of nasal or oral breathing route on upper airway resistance during sleep. Eur Respir J. 2003 Nov;22(5):827-32.
11. Fried R. In: (eds.) Hyperventilation Syndrome: Research and Clinical Treatment (Johns Hopkins Series in Contemporary Medicine and Public Health). 1st ed. The Johns Hopkins University Press. December 1, 1986.
12. Garliner D. Myofunctional Therapy. Philadelphia: Saunders, 1976. Print.(10-12)
13. Guilleminault C, Sullivan S. Towards Restoration of Continuous Nasal Breathing as the Ultimate Treatment. Goal in Pediatric Obstructive Sleep Apnoea. Enliven: Pediatrics and Neonatal Biology. Sept 1st 2014.
14. Jefferson Y. Mouth breathing: adverse effects on facial growth, health, academics and behaviour. General dentist. 2010 Jan- Feb; 58 (1): 18-25.
15. Kim EJ, Choi JH, Kim KW, Kim TH, Lee SH, Lee HM, Shin C, Lee KY, Lee SH. The impacts of open-mouth breathing on upper airway space in obstructive sleep apnoea: 3-D MDCT analysis. Eur Arch Otorhinolaryngol. 2010 Oct 19.
16. Lunn M, Craig T. Rhinitis and sleep. Sleep Med Rev. 2011 Oct;15(5):293-9
17. Lundberg JO. Nitric oxide and the paranasal sinuses. Anat Rec (Hoboken).2008 Nov;(291(11)):1479-84).
18. Lundberg J, Weitzberg E. Nasal nitric oxide in man. Thorax.1999;(54):947-952
19. McKeown,P. Close Your Mouth. Buteyko Books. 2004.
20. Moeller J, Kaplan D, McKeown P. Treating Patients with Mouth Breathing Habits: THE EMERGING FIELD OF OROFACIAL MYOFUNCTIONAL THERAPY. JAOS. 2012 march-april;10-12.
21. Mouth Breathing. The Orthodontists Online Community. nd. accessed January 7, 2015. http://orthofree.com/fr/default.asp?contentID=2401
22. Muliol J, Maurer M, Bousquet J. Sleep and allergic rhinitis. Journal Investigation Allergol Clinical Immunology. 2008;18(6):415-9.
23. Ohki M, Usui N, Kanazawa H, Hara I, Kawano K. Relationship between oral breathing and nasal obstruction in patients with obstructive sleep apnoea. Acta Otolaryngol Suppl. 1996;523:228-30.
24. Okuro RT, Morcillo AM, Ribeiro MÂ, Sakano E, Conti PB, Ribeiro JD. Mouth breathing and forward head posture: effects on respiratory biomechanics and exercise capacity in children. J Bras Pneumol.2011 Jul-Aug; 37(4):471-9.
25. Paskay L. OMD Orofacial Myofunctional Disorders: Assessment, prevention and treatment. JAOS. 2012 march-april; 34-40.
26. Pereira F, Motonaga S, Faria P, Matsumoto M, Trawitzki L, Lima S, Lima W. Myofunctional and Cephalometric Evaluation of Mouth Breathers. Brazilian Journal of Otorhinolaryngology. 2001. 67 (1): 43-49.
27. Schmidt JE, Carlson CR, Usery AR, Quevedo AS. Effects of tongue position on mandibular muscle activity and heart rate function. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:881-888
28. Swift AC, Campbell IT, McKown TM. Oronasal obstruction, lung volumes, and arterial oxygenation. Lancet. 1988 Jan 16;1(8577):73–75.
29. Trabalon M, Schaal B. It Takes a Mouth to Eat and a Nose to Breathe: Abnormal Oral Respiration Affects Neonates’ Oral Competence and Systemic Adaptation. International Journal of Pediatrics. 2012. (207605 ):10 pages)
30. Trawitzki L, Anselmo-Lima W, Melchior M, Grechi T, Valera F. Breast-feeding and deleterious oral habits in mouth and nose breathers. Rev Bras Otorrinolaringol. 2005 nov-dec; 71 (6): 747-51.
31. Antonio Culebras. Long- face syndrome and upper airways obstruction. Sleep disorders and neurological disease. 2005 : 242-243.
32. Keith L. Moore, T.V.N.Persaud, Mark G. Torchia. Development of tongue and upper air ways. The developing human clinically oriented embryology 9th edition .2013; 176-95.
33. John E. Hall, Arthur C Guyton. Tongue posture and swallowing. Guyton and Hall textbook of medical physiology, 12th edition. 2010; 763-765.
34. Golan N, Shahar E, Ravid S, Pillar G. Sleep disorders and daytime sleepiness in children with attention-deficit/hyperactive disorder. Sleep. 2004 Mar 15;27(2):261-6.
35. “ADHD and Sleep.” ADHD & Sleep Problems-National Sleep Foundation. National Sleep Foundation, 2017. Web. 11 Feb.2017. https://sleepfoundation.org/sleep-disorders-problems/adhd-and-sleep.
36. Cortese S, Konofal E, Yateman N, Mouren MC, Lecendreux M. Sleep and alertness in children with attention-deficit/hyperactivity disorder: a systematic review of the literature. Sleep. 2006 Apr;29(4):504-11.
37. Shur-Fen Gau S. Prevalence of sleep problems and their association with inattention/hyperactivity among children aged 6-15 in Taiwan.J Sleep Res. 2006 Dec;15(4):403-14.
38. Valdenice Aparecida De Menezes, Rossana Barbosa Leal, Rebecca Souza Pessoa, Ruty Mara E. Silva Pontes. Prevalence and factors related to mouth breathing in school children at the Santo Amaro project-Recife, 2005. Rev Bras Otorrinolaringol 2006;72(3):394-9.
39. Dillon WC1, Hampl V, Shultz PJ, Rubins JB, Archer SL. Origins of breath nitric oxide in humans. Chest. 1996 Oct;110(4):930-8.
About the Authors
 Martha Macaluso, MLT, RDH, BS, is a practicing Registered Dental Hygienist and Myofunctional Therapist. She received her degree in Dental Hygiene from Farmingdale State University and specialized in Myofunctional Therapy through the AOMT.
Martha Macaluso, MLT, RDH, BS, is a practicing Registered Dental Hygienist and Myofunctional Therapist. She received her degree in Dental Hygiene from Farmingdale State University and specialized in Myofunctional Therapy through the AOMT.
Martha is faculty at New York University College of Dentistry, where she teaches dental hygiene clinic. In addition to her published work, Martha has presented various continuing educational courses in the field of dentistry and myofunctional therapy.
She is extremely involved in the profession acting as editor to the Long Island Dental Hygiene Association, delegate to the Dental Hygienist Association of the State of New York and delegate to the American Dental Hygiene Association.
 Buteyko practitioner and author Patrick McKeown completed his clinical training in the Buteyko Breathing Method at the Buteyko Clinic, Moscow, Russia in 2002 and was accredited by the late Professor Konstantin Buteyko. Patrick has spent the last 15 years working with thousands of children and adults worldwide, who experience breathing pattern disorders, sleep disordered breathing and anxiety. To date, he has written eight books on the subject, and his latest book, The Oxygen Advantage, is an extension of this work, combining specifically-formulated exercises which empower athletes to improve their sports performance.
Buteyko practitioner and author Patrick McKeown completed his clinical training in the Buteyko Breathing Method at the Buteyko Clinic, Moscow, Russia in 2002 and was accredited by the late Professor Konstantin Buteyko. Patrick has spent the last 15 years working with thousands of children and adults worldwide, who experience breathing pattern disorders, sleep disordered breathing and anxiety. To date, he has written eight books on the subject, and his latest book, The Oxygen Advantage, is an extension of this work, combining specifically-formulated exercises which empower athletes to improve their sports performance.




