A Sleepless Nation: What Does The Lack Of Sleep Really Cost Us?
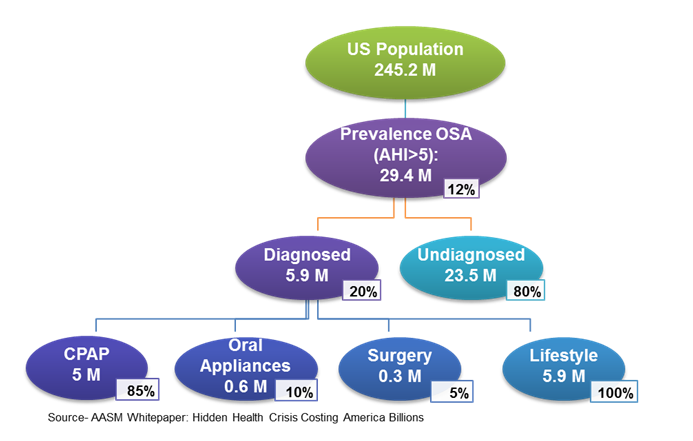
It’s hard to escape the growing amount of research and media attention placed on the importance of sleep. Lack of sleep, both in duration and quality, is being tied to weight gain, comorbidities, anxiety, depression, accidents, earning potential and productivity. A leading mattress retailer even touts the connection between poor sleep quality and chronic pain syndrome on its website. While stress and lifestyle decisions contribute to many people’s sleep problems, there is an under-diagnosed medical condition that affects the sleep of 30 million Americans, obstructive sleep apnea (OSA) (see figure below). OSA is a serious and life-threatening sleep illness that is defined by the American Academy of Sleep Medicine (AASM) as a sleep-related breathing disorder that involves a decrease or cessation in airflow during sleep, despite an ongoing effort to breathe. Other than restless nights and bleary days, what does OSA really cost society as a whole?
Source: American Academy of Sleep Medicine (AASM) Whitepaper: Hidden Health Crisis Costing America Billions
OSA often goes undiagnosed because people with the condition often fail to recognize the symptoms. When OSA symptoms such as drowsiness, fatigue, snoring and poor-quality sleep become the baseline or norm, it can be difficult for doctors and others to explain the need for treatment. Chronic exhaustion causes a strain on the economy since it significantly reduces productivity, exacerbates other healthconditions and increases the risk of motor vehicle and workplace accidents.
The economic burden of undiagnosed sleep apnea among American adults is approximately $149.6 billion in 2015.

The impact OSA has on employers is staggering, with approximately $86.9 billion dollars wasted in lost productivity. Fatigue costs employers billions of dollars in wages for employees whose performance suffers both mentally and physically. In addition, an estimated $6.5 billion in costs are incurred to the economy due to OSA-related fatigue workplace accidents. Drowsiness can reduce reaction time and increase the likelihood of an employee being injured on the job. Other costs associated with this type of accident include lost wages, absenteeism, medical expenses and reduced quality of life. These affect not only the person, but also the employer, healthcare industry and taxpayers.
The research linking OSA to comorbidities such as hypertension, heart disease, stroke, diabetes, depression and anxiety continues to grow. The healthcare utilization costs associated with these physical and mental conditions is approximately $30 billion each year, driven by more hospital and emergency room visits, medication use and, ultimately, mortality rates. The good news is that OSA treatment positively affects mental health and interpersonal relationships.
Motor vehicle accidents in the United States due to sleep deprivation from OSA cost an estimated $26.2 billion in 2015. According to a report by AAA, drowsy driving accounts for nearly 29% of all accidents, but that number may be even higher, as the National Highway Traffic Safety Administration (NHTSA) estimates that more than 10 million accidents go unreported each year. The most visible and highly publicized motor vehicle accidents take place in the transportation industry. With fatigue-related accidents causing millions of dollars in damage and potentially loss of life, there is now a bright spotlight on OSA screening and diagnosis among professional drivers. OSA treatment can reduce costs associated with vehicular damage, medical expenses, lost wages from corresponding absenteeism, property damage and insurance premiums.
Taking on the challenge of underdiagnosed OSA will require commitment from patients, physicians, payors, employers and other stakeholders. One of the most important keys to success is keeping patients already diagnosed with OSA engaged with the CPAP treatment they will likely be using the rest of their lives. ResMed RMD -0.58%’s recently launched myAir app communicates with user’s specialized CPAP machines to monitor and encourage their use. The company reports that myAir users had compliance rates significantly higher than the typical CPAP user. It’s technologies like these and others that will be necessary to deliver the sleep care that tens of millions of American will need now and in the future.
To read more about the effects of underdiagnosed OSA in the United States, read two recently released whitepapers from the American Academy of Sleep Medicine.
This article was written with contribution from Tara Shelton, Consulting Analyst and Charlie Whelan Consulting Director with Frost & Sullivan’s Transformational Health Team TISI +%. For more information on specific needs, challenges or opportunities in the healthcare sector, contact us directly at: TransformationalHealth@frost.com