Undiagnosed sleep apnea caused 2 NYC train crashes. Could you have sleep apnea, too?
Undiagnosed sleep apnea was recently cited as a probable cause in the crash of two New York City commuter trains.
The engineers, who were diagnosed after the crashes, had no memory of the events that killed one person and injured more than 200 others. The National Transportation Safety Board reported that sleep apnea is a probable cause of 10 other highway and rail accidents in the last 17 years, according to the Associated Press.
Sleep apnea is a chronic disorder in which breathing can pause during sleep for a few seconds to minutes — it can happen 30 times or more an hour. The disorder often goes undiagnosed because it cannot be detected during routine doctor visits or by a blood test.
Sleep apnea increases the risk of high blood pressure, stroke, obesity, and diabetes, and is also associated with irregular heartbeats and heart failure. It increases the chances of having a work-related or driving accident, according to the National Heart, Lung and Blood Institute (NHLBI).
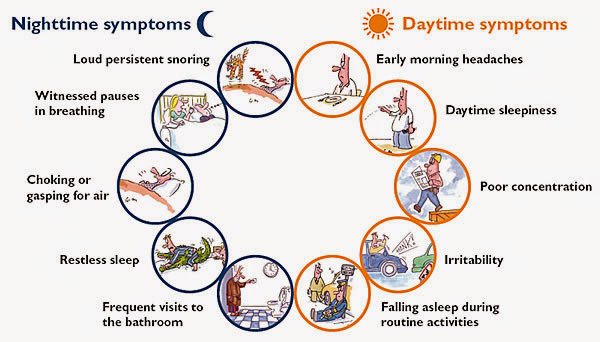
So, how do you know if you have it?
Other signs of the disorder include shortness of breath, gasping for air or choking that wakes you up, insomnia, waking up with a dry mouth or sore throat, a morning headache, attention problems, and irritability, according to the Mayo Clinic.
Men are twice as likely to have sleep apnea as women. Others at risk for the disorder include older adults, anyone with a family history, and people who are overweight, use alcohol, take sedatives or tranquilizers, smoke, or suffer from nasal congestion or narrowed airways.
There are three types of the condition: obstructive, central, and complex.
The most common type is obstructive sleep apnea, when the airway collapses or becomes blocked during sleep and causes shallow breathing or breathing pauses. When air does squeeze by, it can result in snoring. This condition is common in those who are obese, but anyone can have obstructive sleep apnea, including children with enlarged tonsils.
A less common type is central sleep apnea. This occurs when the area of the brain that controls breathing doesn’t send the correct signals to the breathing muscles, and breath stops for brief periods.
When someone has both obstructive and central sleep apnea, it is known as complex sleep apnea syndrome or treatment-emergent central sleep apnea, according to the Mayo Clinic.
It is important to check with a doctor if you suspect you might have sleep apnea. A primary care doctor may refer you to an ear, nose and throat specialist to rule out any blockages in your airways, or a cardiologist, neurologist or sleep specialist, who may recommend overnight monitoring of breathing and other body functions during sleep.
Treatments include using a continuous positive airway pressure (CPAP) machine, which will deliver air pressure through a mask placed over your nose while you sleep. A dentist may recommend an oral appliance designed to open your throat by bringing your jaw forward to relieve mild obstructive sleep apnea.
For extreme cases, a surgeon may perform an uvulopalatopharyngoplasty, in which tissue from the rear of the mouth and top of the throat, as well as tonsils and adenoids, are removed.